Hospitals & ICE: What You Need To Know
Are hospitals and medical clinics becoming battlegrounds in the ongoing immigration debate? Recent policy shifts and enforcement actions suggest a disturbing trend: the potential for healthcare facilities to be targeted in immigration raids, jeopardizing patient care and eroding trust within vulnerable communities.
The landscape of immigration enforcement is shifting, and the implications for healthcare providers and their patients are profound. For years, places of healing, like hospitals and medical clinics, were largely considered "sensitive locations," shielded from routine Immigration and Customs Enforcement (ICE) operations. This protection, established by the Obama administration, aimed to ensure that individuals, regardless of their immigration status, could access necessary medical care without fear of detention or deportation. However, recent developments have drastically altered this landscape, raising serious concerns about the future of healthcare access and the safety of both patients and healthcare workers.
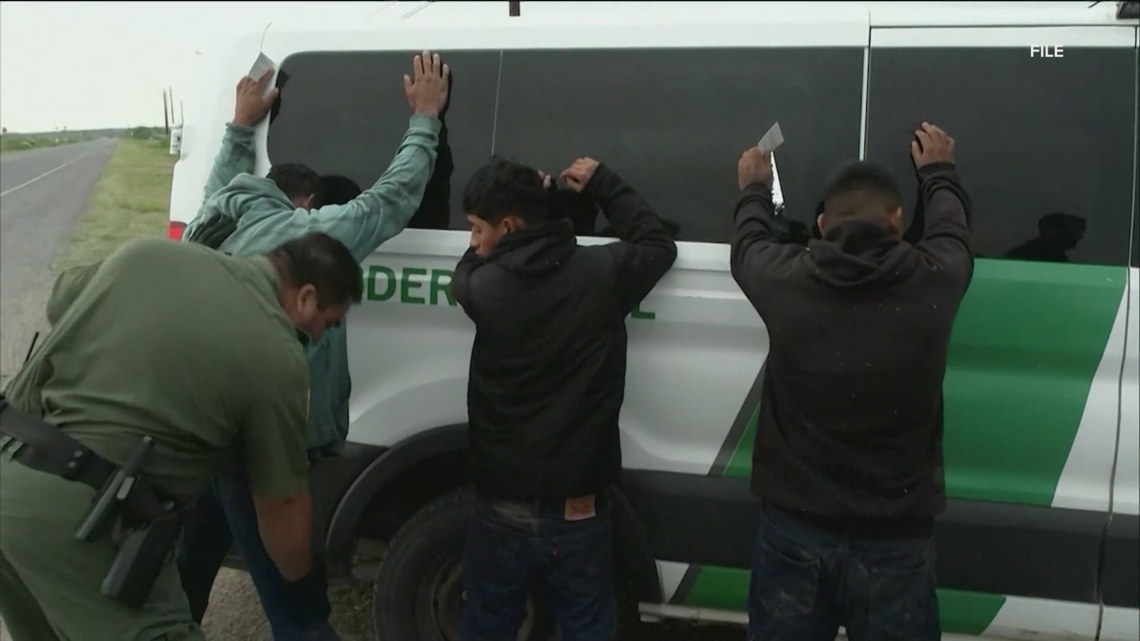
The Trump administrations decision to rescind the policy protecting "sensitive areas" including churches, schools, and hospitals has opened the door for increased ICE presence in these traditionally safe spaces. This policy reversal, coupled with reports of ICE agents detaining patients and targeting individuals visiting sick family members, has created an atmosphere of fear and uncertainty within immigrant communities. The potential for raids within hospitals and clinics not only disrupts the delivery of medical care but also undermines the trust patients place in healthcare providers, leading to reluctance to seek medical attention when needed.
The implications of this shift are far-reaching, extending beyond the immediate risk of detention and deportation. The presence of ICE agents in healthcare facilities can intimidate patients, deterring them from seeking vital medical services. This is particularly concerning for vulnerable populations, including children needing emergency care and individuals with chronic illnesses. Furthermore, healthcare providers are now placed in precarious positions, grappling with the need to balance their legal obligations with their ethical duty to provide care to all patients, regardless of immigration status. The erosion of trust and the potential for disruption of care pose a serious threat to public health.
The implementation of "ICE drills" and the creation of internal protocols, as seen in some organizations, reveal the growing anxiety of healthcare workers and the measures they're taking to navigate the new environment. Healthcare providers are tasked with navigating a complex web of legal requirements while simultaneously trying to maintain a safe space for patients. The guidance issued by institutions like NYU Langone and NYC Health + Hospitals are examples of the steps being taken to clarify institutional responses, but the fact that these guidelines are necessary underscores the challenges presented by the evolving enforcement landscape.
The recent developments have not only raised ethical and moral questions but also ignited a debate about the role of healthcare providers in the immigration process. The question of whether medical professionals should be required to cooperate with ICE, share patient information, or even assist in detaining individuals is at the forefront of this discussion. The potential for federal immigration enforcement to seek information about patients, staff, and visitors further complicates the situation, forcing hospitals to balance their commitment to patient confidentiality with the demands of law enforcement.
In response to these changes, healthcare providers are implementing proactive measures to protect their patients and staff. These steps include designating a point of contact (POC) to manage ICE inquiries, establishing clear protocols for documenting ICE interactions, and training staff on how to respond in the event of a raid. The goal is to create a safe and welcoming environment where patients can receive the care they need without fear of immigration enforcement.
Here's a look at the key aspects of the shifting policy and practical guidance for healthcare providers:
| Issue | Description |
|---|---|
| Revocation of "Sensitive Locations" Policy | The Trump administration rescinded a policy that protected sensitive areas like hospitals, schools, and churches from ICE raids. This has led to increased apprehension of people within these locations. |
| ICE Operations in Healthcare Facilities | ICE agents have been reported to remove, detain, or apprehend patients in medical facilities. Children needing emergency care and family members of sick patients have been targeted. |
| Impact on Healthcare Providers | Healthcare employers and workers are put in difficult positions. They must balance patient care with legal compliance and ethical responsibilities. |
| Public Health Concerns | Allowing ICE raids in healthcare settings is seen as a potential public health crisis, likely to deter people from seeking medical help. |
| Increased Anxiety | Healthcare workers have expressed heightened anxiety due to increased immigration enforcement and the potential for ICE presence. |
The 4th Amendment to the U.S. Constitution provides some protection. ICE generally needs a judicial warrant to enter the private spaces of hospitals (like patient areas) or schools. However, the changing policies and enforcement practices mean that these protections are continually tested and may not always suffice to provide sufficient safety.
Many healthcare providers are also developing the following protocols to manage the risk:
- Designate a Point of Contact (POC): Assign a specific person to manage ICE inquiries and coordinate staff responses.
- Develop Clear Protocols: Establish and communicate clear guidelines for documenting ICE interactions and preserving patient confidentiality.
- Professional Interactions: Greet ICE agents professionally, request identification, and inquire about the purpose of their visit.
- Staff Training: Conduct "ICE drills" and provide training to educate staff on what to do in the event of a raid.
- Legal Review: Consult with legal counsel to clarify your rights and responsibilities in these situations.
- Community Outreach: Communicate with the local community about the hospitals policies and commitment to patient safety.
- Patient Support: Offer support and resources to patients who may be affected by ICE actions, including legal aid and counseling services.
- Policy Review: Continuously review and update your policies and procedures to align with the latest legal and enforcement developments.
The recent changes in immigration enforcement highlight the importance of having robust and well-defined policies and protocols in place to address this issue. Healthcare providers should be prepared to navigate this complex and evolving landscape, prioritize patient safety and confidentiality, and work to uphold their ethical and legal obligations.
The revocation of the "sensitive locations" policy is a pivotal moment in the ongoing dialogue between immigration enforcement and healthcare access. This action has far-reaching implications, transforming the environment within healthcare facilities and placing healthcare providers on the front lines of this complex issue. The potential chilling effect on healthcare access is a grave concern that must be addressed by healthcare facilities, legal professionals, and policymakers alike. Healthcare providers are now tasked with navigating a complex web of legal requirements while simultaneously attempting to maintain safe spaces for patients.
The strategy of targeting migrants as they exit hospitals and medical centers has prompted concern from healthcare workers about where and when federal agents can enter a facility for enforcements, leading some organizations to create training and ICE drills to help staff and providers know what to do in the event of a raid.
The removal, detainment, or apprehension of immigrant patients from medical facilities, including children needing emergency care and immigrants visiting sick family members, can create a chilling effect, deterring immigrants from seeking necessary medical attention. This creates challenges for healthcare providers as they seek to provide medical care in an environment of distrust and fear. The increased enforcement has raised serious concerns among healthcare workers about patient privacy and the potential for adverse impacts on public health.
In New York, for example, the city's public hospital system, Health + Hospitals, is likely to be most impacted by ICE raids, given its position as a safety net provider serving a large population. Healthcare providers must implement the following:
- Create clear guidelines about how to interact with ICE agents.
- Ensure that staff members are informed of the organization's policies.
- Provide training to ensure that staff members understand their rights and responsibilities.
- Develop protocols for handling patient information requests.
- Safeguard patient confidentiality.
- Consider providing legal resources for patients impacted by immigration enforcement actions.
The shift in policy and its consequences have drawn attention to the critical role that healthcare providers play in promoting public health and trust within communities. The creation of safe spaces is essential for ensuring that all individuals can access necessary medical care without fear of discrimination or deportation. As the landscape of immigration enforcement continues to evolve, healthcare providers must proactively protect their patients rights and create an environment in which everyone feels safe.
The steps taken by healthcare providers, such as assigning a point of contact for ICE inquiries and establishing clear protocols for documenting interactions, are essential components of a comprehensive approach to addressing the impact of these policy changes. Through these efforts, healthcare providers can safeguard patient confidentiality, create a safe environment for care, and advocate for the rights of all patients, regardless of their immigration status. The key is to protect the access to healthcare for all.